What is the problem?
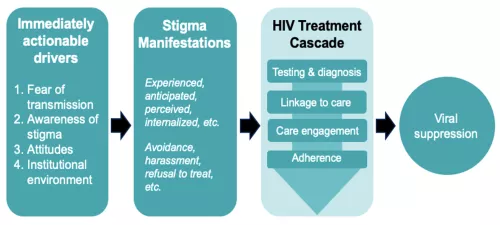
HIV-related stigma and discrimination (S+D) in healthcare settings is a significant barrier to the achievement of UNAIDS’ 95-95-95 targets, discouraging people living with HIV (PLWH) and key populations (KP) at high risk of HIV acquisition from engaging in care and prevention services and negatively impacting their adherence to life-saving treatment (Figure 1). In the Asia/Pacific region, the HIV epidemic is highly concentrated among KPs of men who have sex with men, sex workers, transgender people, and people who inject drugs. The HIV-related S+D they experience is further compounded by cultural, social, and institutional factors that discourage care-seeking, undermine treatment self-efficacy, and normalize marginalization. Thus, addressing S+D is critical to reaching these KPs and ensuring they receive HIV prevention and treatment services responsive to their unique identities, needs, and circumstances.
Validated tools and evidence-based interventions exist to measure and reduce HIV-related S+D. Yet, their incorporation into routine programming in Asia/Pacific remains limited for many reasons and reflects the inherent difficulty of scaling pilot projects to generate population-level impact. Previous initiatives to reduce S+D in the region have assumed that training alone – and episodic rather than continuous measurement of its prevalence – is sufficient to eliminate S+D in healthcare settings. Training is necessary to remedy gaps in knowledge that perpetuate S+D; however, it does not address other factors through which S+D is produced and abetted, nor does it assure gains in knowledge are translated into practice. As the drivers of HIV-related S+D are multi-dimensional and highly contextual to the locale, so, too, must be the interventions aimed at reducing S+D.